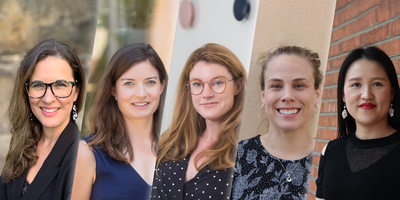
Meet Dr Xia Wang, Doctoral Research Fellow, Neurological Program
Dr Xia Wang is a Doctoral Research Fellow at The George Institute for Global Health specialising in the analysis of large-scale randomised controlled trials and conducting epidemiological studies.
Tell us a little bit about yourself. What were your motivations for getting into research, specifically stroke research?
Stroke is the leading cause of death in China, with the country accounting for roughly one third of the world’s stroke mortality. In the northern rural area where I grew up, the burden of stroke is much higher compared to other parts of China.
The prevalence of major risk factors for stroke remains high - salt intake is much higher; tobacco use is highly prevalent; levels of awareness, treatment, and control of hypertension and diabetes are all low. After a stroke, the quality of care and secondary prevention are sub-optimal therefore rates of recurrent stroke are higher.
I was motivated to get into stroke research as I believed it could help me understand why this was the case and what I could do to help tackle this monumental challenge in my home town.
Can you tell us a little bit about your latest research?
One key area I have been researching is sex differences in stroke. We found that women who had ischemic stroke (a lack of oxygen supply caused by the blockage of a blood vessel) had better survival rates but were also more disabled and had a poorer quality of life afterwards. We also found that women had a poorer prognosis than men which worsened with age after acute ischemic stroke.
Another area of my research is focusing on patient-centered outcome measures. Usually in stroke research and clinical practice the most commonly used measures of functional status don’t adequately capture the broader impact on overall wellbeing. I found stroke patients’ views of health and wellbeing differ across levels of disability but larger improvements in quality of life can generally occur as they become less severely disabled and more independent. More patient-centered outcome measures can better capture patients’ health perceptions and well-being compared to the traditional functional outcomes used in acute stroke trials.
What inspired you to join The George Institute for Global Health?
I was fascinated with the many amazing randomised controlled trials conducted at The George Institute. It was a dream come true to attain a PhD in Australia and through working with Professor Craig Anderson I got the opportunity to join The George Institute full time. It has been an enjoyable journey so far and working here has been a major milestone in my professional life.
You were recently awarded a coveted NHMRC grant for your project “Generating new evidence to better guide stroke management”. Can you tell us a little bit about how the process for applying for this grant works and why perseverance is important?
Learning from the application process is the key thing for me. It’s important to treat the entire process of applying for grants as an educational opportunity. The success rate of grant applications is relatively low - it’s normal to fail, so focus on the application itself when working on it regardless of the outcome. One key piece of advice I would give to anyone applying for a grant is to give yourself plenty of time to write it and then rework it based on feedback from colleagues and advisors.
What is your favourite part of being a Doctoral Research Fellow?
I’ve been given so many opportunities for self-improvement through working at The George Institute as a Doctoral Research Fellow. I have also been lucky enough to have several talented senior mentors around me who have guided me and allowed me to better myself.
What other roles do you have?
I am also working with colleagues from low- and middle-income countries on various other stroke studies. For example, I am currently collaborating with colleagues on stroke incidence studies in Mongolia where the high prevalence of elevated blood pressure is causing a greater stroke burden