‘Every action matters, every bit of warming matters, every year matters, every choice matters’ Prof Kristie Ebi, University of Washington
On 5 and 6 December 2019, I joined Professor Ebi and others as a participant at the Symposium of Climate Change and Health, hosted by the Swiss Tropical and Public Health Institute in Basel, calling for global thinking and local action.
At the time of writing, there are only 25 sleeps to go before we enter a new decade. Looking back over 2019, we have witnessed a surge in public awareness of, and campaigns to protect, the health of our planet, as reflected by Collins Dictionary naming ‘climate strike’ their Word of the Year.
The term ‘climate change’ is often used interchangeably with ‘global warming’ to signal the effects of excessive emissions of greenhouse gases such as carbon dioxide, to which the main contributor is the combustion of fossil fuels, e.g. coal and oil. If we continue with ‘business-as-usual’ without firm actions to stall such change, we will see more extreme climate-related events at a greater frequency and intensity, the world over in the next 10 years. The threat this poses to the health of every species, including humans, of this planet, cannot be understated.
Climate-related health risk
Climate change poses major risks to health globally. Some vector-borne diseases (e.g. malaria, dengue) are highly sensitive to increased temperature or rainfall, which ultimately affects vector distributions and the ecosystem as a whole. These diseases are disproportionately affecting populations in tropical countries.
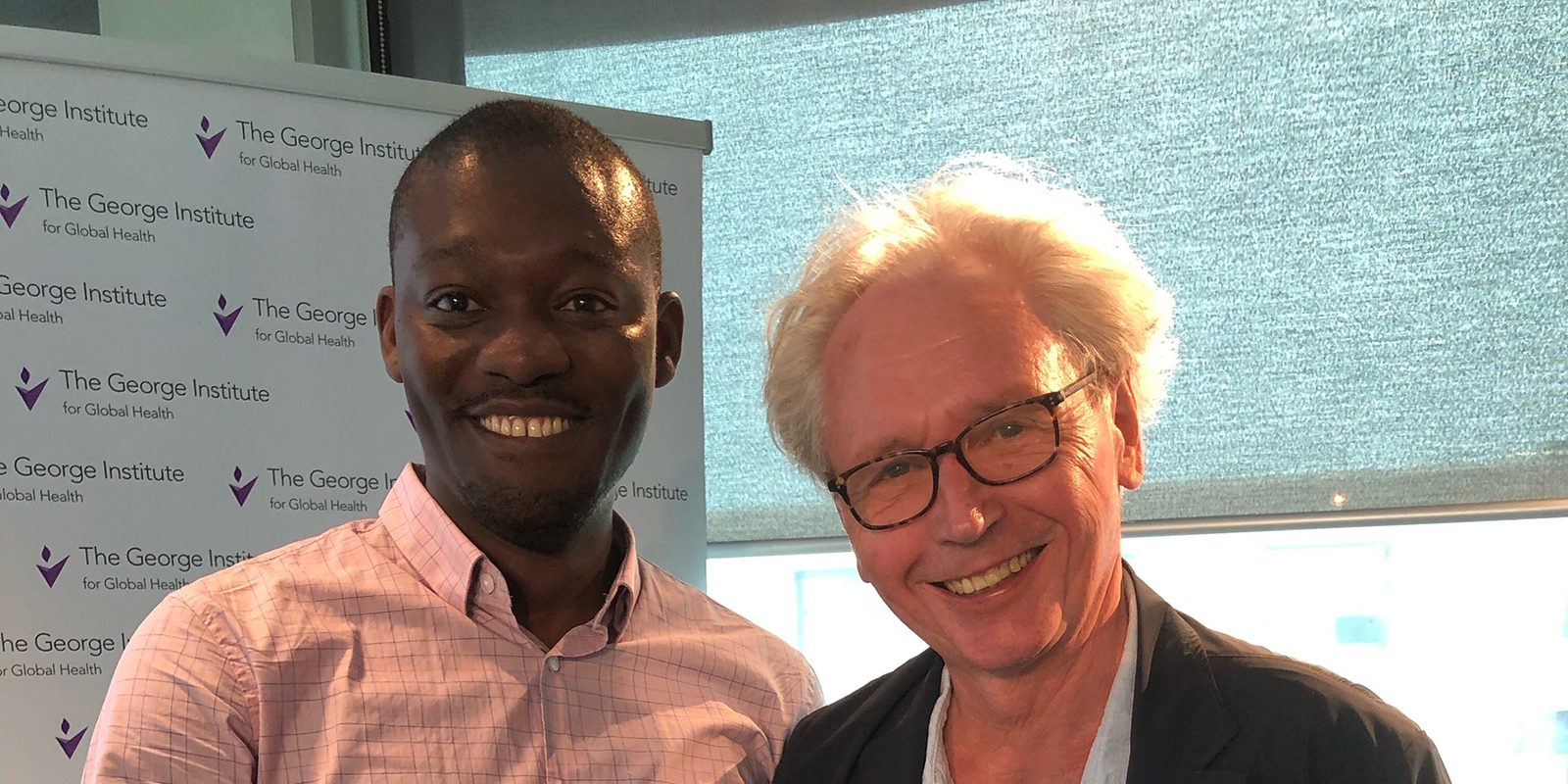
Non-communicable diseases (NCDs) relating to climate change are also being increasingly studied, as in my work with PEAK Urban as a researcher with The George Institute for Global Health at the University of Oxford. Alarming evidence is emerging that climate change not only reduces overall crop yields, but also depletes nutritional quality in terms of reduced iron, zinc and many other micronutrients. This carries significant impacts on long-term population health through possible malnutrition. The complexity, prevalence and reach of chronic mental health conditions are also posing significant burdens on the global community. For example, flooding has been associated with anxiety in affected communities while increased temperature seems to be linked to an increased suicide rate in this multi-city study.
Climate change can also impact health through social factors, for example, climate-related migration. This complex and context-specific issue is a focus of by the Informal Cities project team which looks at the socioeconomic and geopolitical drivers of migration, urbanisation and health. Symposium discussions also underscored the major injustice faced by individuals and communities in the Global South. Such populations are likely contributing the least to this climate crisis, but are currently paying the greatest price for it with immense challenges to combat climate change while urbanisation shifts the environmental and social face of nations burdened with infectious and non-communicable disease, and in the absence of strong investment in sustainable, climate-sensitive infrastructure. Recent floods in east Africa claimed lives and affected hundreds of thousands more. It is crucial that wealthier countries in the Global North re-examine and firmly implement their climate-related policies such as ceasing the sale of the poorest possible quality diesel to Africa (containing up to 630 times more sulphur than diesel sold in Europe). So too, it is crucial to work collaboratively to close data gaps; one of which I am working on with PEAK Urban colleagues as we investigate the role of broader environmental factors on children’s respiratory health across all sub-Saharan African countries.
Resolving to put health at the heart of climate action
Where there is risk, there is opportunity. The health-related benefits that would result from mitigating the progression of climate change are substantial. For instance, policies targeting short-lived climate pollutants (e.g. black carbon, ozone) in local areas can strongly contribute to cleaner air and better health, a justified motivator of near-term actions for all stakeholders.
In the wake-up call of this climate crisis, healthcare systems should take the opportunity to move towards smart and climate-resilient healthcare, which is particularly important for the most vulnerable regions.
Symposium participants were asked ‘what is the most important mitigation measure that individuals can take to reduce [their] carbon footprint?’. Responses included: minimising air travel; eating less meat; consuming less; reducing reliance on car travel – why not resolve to adopt one or more as 2020 dawns the future awaits. Now is the time to act.