George Institute researchers have secured funding totalling over three million dollars (Australian) to improve the health and wellbeing of adolescents living in slums in India and school children in Fiji. The funds will be split across two research projects, led by Prof David Peiris and Dr Bindu Patel respectively.
The funding has been awarded by The Global Alliance for Chronic Diseases (GACD), which brings together national and international funding agencies to address non-communicable diseases (NCDs) in low- and middle-income countries (LMICs) and vulnerable populations in high-income countries (HICs). It focuses on implementation research that takes a life course approach to preventing and reducing common NCD risk factors.
Australia’s National Health and Medical Research Council (NHMRC) is one of the funding agencies in the GACD.
Building resilience in urban slums
Prof David Peiris, Director of the Institute’s Better Care Program, and Prof Pallab K. Maulik, Deputy Director in the George Institute India will lead a multidisciplinary research consortium from India and Australia to implement a life-skills program for young people living in Indian urban slums.
The project, named ANUMATI - which means ‘consent or permission to do something’ in Hindi - will involve older adolescents (15-19 years) with or at high risk of depression living in New Delhi and Hyderabad. It will include a 16-week education program delivered by trained facilitators and a peer-led social media program. The project aims to reduce depression symptoms, and other non-communicable disease (NCD) risk factors like smoking, alcohol consumption, and substance abuse and to test whether low-cost social media programs perform as well as in-person education programs.
Prof Peiris says, “With the ANUMATI implementation study, we are widening our focus from health care sector specific interventions to community-based approaches to enhance young people’s resilience. We have seen these approaches work in different parts of the world and hope to apply those learnings to improve the wellbeing of young people living in challenging environments such as slums.”
The four-year project begins in October 2023.
Preventing disease through health promotion in schools
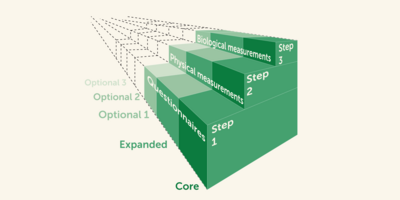
Dr Bindu Patel, Senior Research Fellow in the Health Systems Science team at The George Institute, has secured funding to assess the effectiveness of Health Promoting Schools (HPS), a national government-supported program in Fiji. Launched in 2016 by Ministry of Education, Heritage and Arts (MEHA) and Ministry of Health and Medical Services (MHMS), HPS is a cross-sector program delivered through the school curriculum to improve health and wellbeing by addressing common risk factors for NCDs.
The goal of this research project is to evaluate the impact of the program so far and assess the value in scaling it up in Fiji. It will be conducted in partnership with MEHA, MHMS, and Fiji National University.
Explaining the potential impact of this work, Dr Patel says “Effective and sustainable systems level changes can only be made through multi-sectoral approach to health promotion, and continuous information gathering and feedback to adapt interventions. Our evaluation will inform HPS implementation strategies to optimise health, educational and social outcomes for different groups across the Fijian community.”
The project will start in July 2023 and run over a period of five years.