New research highlights need for urgent action
Our latest research studying the burden of stroke in Mongolia has found that it affects a much younger population compared to high-income countries (HICs). It occurs at a mean age of 60 years, which is at least ten years earlier than the average age in HICs.
The study, published in The Lancet, is a collaboration between The George Institute for Global Health and the Institute of Medical Sciences in Mongolia. Covering half the country’s population across six large districts in the capital city of Ulaanbaatar, this is a first-of-its-kind population-based study detailing the burden of stroke in the country.
Lead author, Associate Professor Chimeglkham Banzrai, who heads the Department of Neurology at the Mongolian Institute says, “Collecting reliable data is the first step in planning an effective response to a health challenge. That’s where the impact of our study lies – this evidence can inform Mongolia’s strategy on stroke management and help prevent many premature deaths and disability.”
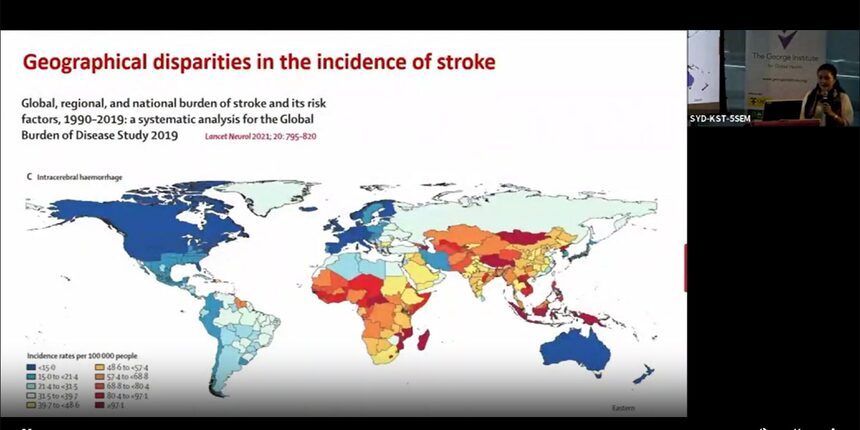
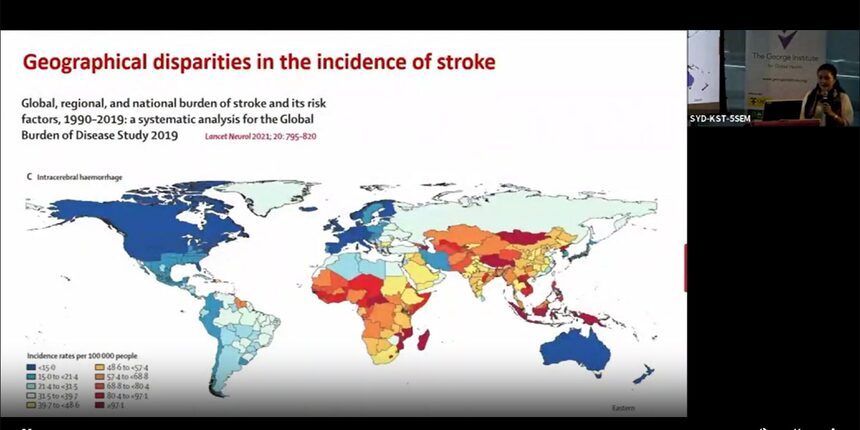
Apart from highlighting the age disadvantage, the study also revealed that the incidence of haemorrhagic stroke – caused by bleeding into the brain from a ruptured blood vessel - is several-fold higher in Mongolia than anywhere elsewhere in the world. Also, the outcome for stroke is extremely poor in the country - at least one third of the stroke cases result in death within 28 days, and over two thirds in death or significant disability within a year.
A/Prof Banzrai explains the possible reasons behind the severity of the problem. “There is a high prevalence of hypertension compounded by poor recognition, treatment and control of elevated blood pressure - high salt intake being a major factor. According to the WHO, the average daily intake of salt in Mongolia is 10.5grams - more than double the recommended level.”

The WHO recommends cutting salt intake by 25 percent by 2025 as part of efforts to reduce the burden of non-communicable diseases like stroke. But challenges related to policy implementation and gaps in industry engagement are major barriers to achieving this. And they are especially relevant in low and middle-income countries like Mongolia.
“Apart from this, a diet low in fruit and vegetables, growing rates of obesity and environmental factors like high levels of air pollution, and extreme weather conditions only add to the risk factors in the country,” she adds.
The main cause of death in Mongolia is ischaemic heart disease, with rates double the global average estimates. Ischaemia or ischemic heart disease is a condition in which the heart is starved of oxygen due to a reduced blood supply when vessels become blocked. Stroke is the next most common cause of death, with rates in the country at least double those of other low-middle income countries. It is also the leading cause of disability in Mongolia.
“The high burden of stroke in the country highlights the need for urgent action at the highest level. We hope the findings of our study can be used to inform implementation of programs, the scale-up of activities for primary and secondary prevention, and better organisation of health services related to stroke,” she concludes.
The study, which began in 2019, was approved by the Government of Mongolia but lacked sufficient funding to be completed. The Global Brain Health Initiative at The George Institute, led by Professor Craig Anderson, stepped in to partner and invest in the study.
“Our program aims to address the serious issue of brain health and get people living better for longer. We want to work collaboratively with researchers all around the world, especially those in countries where the burden of ill health is the highest. Achieving health equity is key to the George Institute’s mission,” says Prof Anderson.